Poor mental health may be another symptom of malnutrition
In a nutshell
Very low carbohydrate, ketogenic diets improve mental health
Strong evidence shows that mental illness is a symptom of poor metabolic health
Pharmaceutical drugs designed to treat mental illnesses contribute to their root cause
This article is based on the presentation by Dr. Rachel Brown at the First Annual Keto Brain Health Conference. Dr. Brown is a psychiatrist with 20 years’ experience and I first came across here work at the Public Health Collaboration Annual Meeting 2024 in May.
I’ve tried to summarise her talk here in ways that a lay-person like me can understand what she was describing. I haven’t followed up on any of the references she provided. However, each of the points I’ve summarized below are supported by references to the academic literature.
Incidentally, I recorded the details of her slides using my iPhone camera and used those images to recreate her message here. Where would we be these days without pocket-sized technology?
Causes of mental health issues
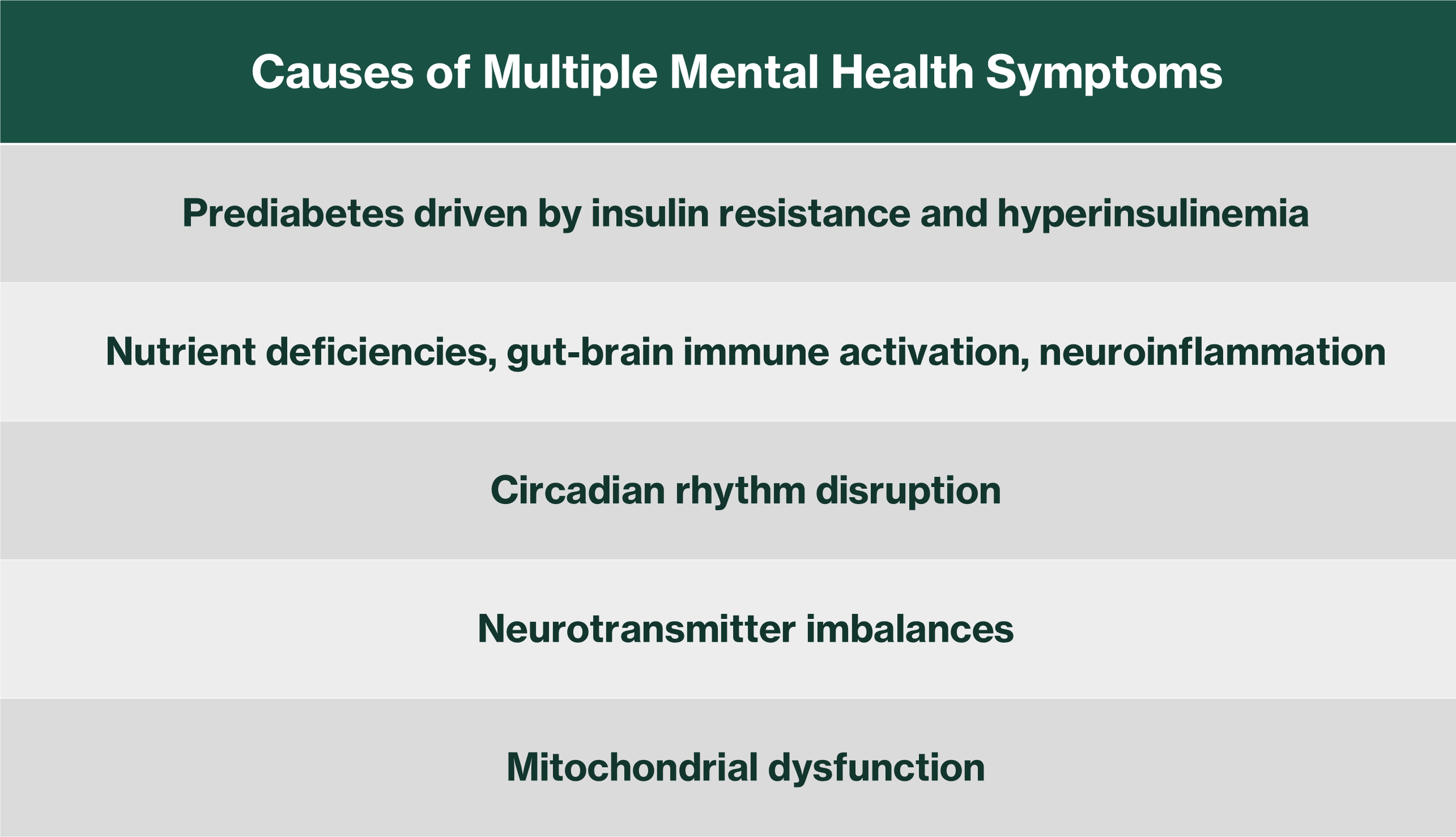
Dr. Brown described several causes of mental health disorder related to poor human metabolism (Table 1). Note that none are described as chemical imbalances.
Table 1: Root causes leading to chronic inflammation associated with mental health
Chronic inflammation associated with each of the causes in Table 1 is a common factor. This comes from evidence of raised biochemical markers of inflammation in people with depression.
Depression
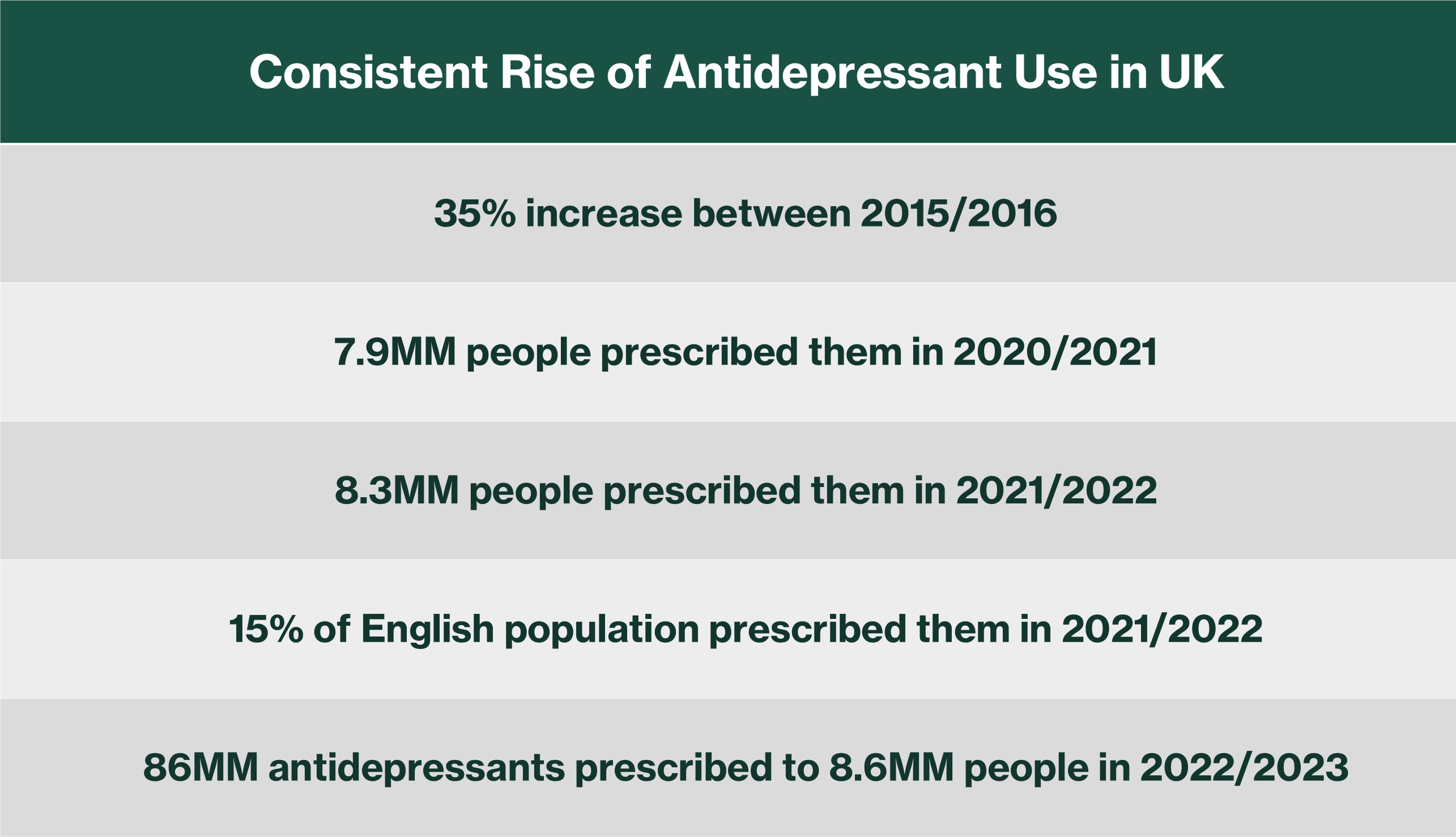
Dr. Brown spent more time describing the literature on depression than other mental health disorders. The incidence of depression in the UK is a major health issue and it is rising annually (Table 2).
Table 2: Antidepressant use in the UK is high and rising every year
The academic literature contains many references to links between obesity, type 2 diabetes (both caused by poor metabolic health associated with processed sugar and starch) and depression. The findings of the underlying research often agree with each other (which means that they are more likely to be correct), hence the apparent overlap of the statements that follow.
Obesity
Obesity and depression are inflammatory disorders
Obese people have a 55% increased risk of developing depression
A significant positive association between depression and obesity has been observed, and it is stronger in women than in men
Obese individuals are twice as likely as non-obese to experience clinical depression
Type 2 Diabetes
Depression is a risk factor for the onset of type 2 diabetes
Type 2 diabetes is a risk factor for depression
People with depression have a 35% increased risk of developing diabetes
Depression appears in 10% to 15% of type 2 diabetics…twice the rate in non-diabetics
Other mental health issues
Obesity
In a study of 18-25 year old German women, obesity was associated with increased risk of mood and anxiety disorders
Obesity is associated with a 25% increase in the probability of mood and anxiety disorders
Type 2 diabetes
People with schizophrenia are two to five times more likely to develop type 2 diabetes than non-schizophrenics
People with bipolar disorder and schizophrenia show a 33% increased risk of type 2 diabetes compared to non-sufferers
Metabolic syndrome
Metabolic syndrome is an inflammatory state with alteration of inflammatory markers
The incidence of metabolic syndrome is higher in people with bipolar disorder compared to those that are unaffected
US - 36% to 49% vs 32% in general population
Europe – 19% to 27% vs 8% to 17% in general population
Pharmaceutical drugs are not the answer
Antidepressants
Drugs used to treat depression are associated with obesity and type 2 diabetes compared to people not on those drugs
Tricyclic antidepressants – almost twice the risk
SSRIs – twice the risk
Lower doses and shorter-term use are not associated with increased T2D risk
Cause measurable weight gain
4% to 25%
5% to 10% of treated people gained 7% or more of body weight
Mirtazipine used for 20wk – 13% gained weight
Amitriptyline for 20wks – 22% gained weight
Tricyclics increase preference for sweets
Emotional blunting/numbing common - 70% affected by longer term use
Drugs for other conditions
Mood stabilisers are associated with higher insulin, weight gain, and increased body mass
Second-generation antipsychotics are associated with weight gain
Drugs for schizophrenia have been associated with food addiction
Drugs used to treat bipolar disorder cause insulin resistance, increase the risk of type 2 diabetes, and the risk of developing metabolic syndrome
Diet Matters
Certain mental health issues are associated with dietary gluten and can be resolved with a gluten-free diet
Bipolar disorder patients have been shown to be reacting to wheat products during acute episodes
The ketogenic diet
A ketogenic diet reverses high insulin and inflammation
Lowering insulin addresses insulin resistance and hyperinsulinemia
This is anti-inflammatory, reduces oxidative stress and restores brain chemical balance
Ketones are protective for brain
Ketosis can prevent and reverse production of excess brain chemical messengers (glutamate)
Excess glutamate production is implicated in development of mental disorders
A ketogenic diet promotes protective brain immune cells (microglia)
Now that Dr. Brown has raised the subject, let’s remind ourselves what that means.
What is a ketogenic diet?
I always rely on the excellent book on the subject published by Tim Noakes’ Nutrition Network. The book describes a ketogenic diet as a therapeutic diet of very low carbohydrate (e.g., sugars, starches, grains) content which induces the production of ketones as a source of fuel for the body. They state (p.72):
“The ketogenic [ketone forming] threshold is the level of daily carbohydrate intake at which there is an increase in measurable ketone production in the blood, urine and/or breath. This ketogenic threshold is variable , but the percentage of individuals with an elevation in ketones increases as the amount of carbohydrate in the diet decreases. When the daily total carbohydrate intake is below 20g per day, nearly everyone will have an elevation in ketone concentrations. This elevation in measurable ketones is called nutritional ketosis”
I also addressed this in my summary of the 2024 PHC Annual Meeting when I reproduced a graphic by Dr. Anthony Chaffee (Figure 1). It shows that low carbohydrate, ketogenic, and carnivore are subsets of real nutrient-dense food and represent increasingly restricted sources of carbohydrate:
Figure 1: Low carbohydrate, ketogenic, and carnivore diets are all subsets of nutrient-dense real food
Comparing the ketogenic diet to pharmaceutical drugs
When we compare the effect of a ketogenic diet with the effect of common pharmaceutical drugs on the root causes of poor mental health (Table 1), the results are remarkable (Table 3).
In mental health patients, a ketogenic diet reduces the underlying insulin resistance and chronic inflammation. This in turn improves metabolic health as manifest in the body’s powerhouses (mitochondria), brain energy improves, and associated symptoms such as type 2 diabetes and immune function are eliminated.
Pharmaceutical drugs, designed to treat the chemical imbalances that result from root-cause poor metabolic health, have the opposite effect of a ketogenic diet. They have been shown to lead to insulin resistance and the progression of associated symptoms of metabolic dysfunction such as type 2 diabetes, heart disease. If that isn’t bad enough, they are associated with persistent sexual dysfunction and cause withdrawal symptoms when patients try to get off them.
Table 3: A ketogenic diet reduces and pharmaceutical drugs contribute to the root causes of mental health
Summary
I have previously described how consuming too much sugar and starch raises blood insulin. When this occurs consistently over a long period of time, the body develops insulin resistance. The combination of insulin resistance and constantly raised insulin constitute poor metabolic health which over time leads to things like obesity, heart disease, type 2 diabetes, raised blood pressure, non-alcoholic fatty liver, poly-cystic ovarian syndrome (PCOS), etc. Whilst these conditions are described as forms of chronic disease, they are, in my opinion, symptoms of consuming too much processed sugar and starch.
It should also be noted that those symptoms often co-occur. In other words, obese people are often diabetic or suffering from heart disease, for example.
It appears to me from Dr. Brown’s work that common forms of mental illness are also more likely symptoms of poor metabolic health, rather than obviously separate diseases. This is also the conclusion of Dr. Chris Palmer. In his excellent book, he describes mental illness as metabolic disorder, and not diseases of chemical imbalance.